The American Academy of Dermatology (AAD) has published new guidelines of care for the management of adult and pediatric atopic dermatitis. Published in the Journal of the American Academy of Dermatology (Part I in February 2014 and Parts II and III published online, May 7, 2014), these evidence-based guidelines focus on treatment options for milder versions of this skin condition as well as more serious cases that have not responded to other approaches.
“Dermatologists work very closely with patients, or with parents of patients, to determine the most effective and soothing treatments for this dry and itchy skin condition,” said board-certified dermatologist Brett M. Coldiron, MD, FAAD, president of the AAD. “These guidelines provide valuable recommendations for both patients and dermatologists for identifying and utilizing the best treatment options depending on the severity of the patients’ disease and its impact on their quality of life.”
First Line Therapies
For patients with atopic dermatitis, the following are recommended as first-line therapies:
- Moisturizers are an essential part of treatment for patients with atopic dermatitis, even those with moderate and severe atopic dermatitis. Patients should choose a moisturizer that is free of additives, fragrances, and perfumes, and is in the form (e.g. cream, ointment, oils, gels and lotions) that they prefer and will use regularly.
Since there is currently not any scientific evidence that demonstrates how often to apply moisturizer or how much to apply to achieve optimum benefits, patients should apply and reapply as much moisturizer as they feel is necessary to achieve relief. Moisturizers should be applied after bathing. - Bathing. While there is little evidence to support a standard bathing frequency or duration, it is generally suggested that patients bathe up to once a day, for five to 10 minutes in warm water, followed by moisturizing. Patients should use non-soap cleaners that have a neutral to low pH, are hypoallergenic and fragrance-free.
Bleach baths are recommended when there are visible signs of infection. A patient’s dermatologist can provide guidance and instructions on when bleach baths may be effective. - Wet wrap therapy is recommended to quickly reduce patients’ atopic dermatitis flares. Wet wraps help increase the penetration of moisturizers and prescription topical medications, decrease water loss, as well as provide a physical barrier against scratching.
To apply a wet wrap, patients moisturize their skin, and then wrap the skin in a layer of wet bandages. A layer of dry bandages is then applied over the wet bandages. - Topical corticosteroids (TCS) can be used to treat active inflammation and itch, and to prevent future disease flares.
- Topical Calcineurin Inhibitors (TCI) may be prescribed for patients with atopic dermatitis who have not found relief through first-line treatments, such as moisturizing, bathing, wet wrap therapy or TCS, or when the use of TCS is not advisable. TCI include tacrolimus or pimecrolimus. Patients, including those under two years of age, can use this treatment off-label under the guidance of their dermatologist.
“While the FDA has placed a black box warning on TCI stating that there is a lack of long-term safety data about the potential risk of cancer, such as skin cancer and lymphoma, patients should know that studies have not demonstrated an increased cancer risk from TCI use,” said dermatologist, Lawrence F. Eichenfield, MD, FAAD, one of the authors of the Academy’s newest guidelines of care. “Patients and parents of patients can talk with their dermatologist about concerns with the use of this medication.”
[pagebreak]
Severe Atopic Dermatitis
For patients with severe atopic dermatitis who have been unable to control their symptoms using first-line therapies, the guidelines recommend:
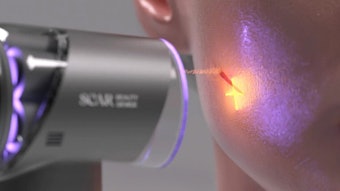
- Phototherapy. Ultraviolet (UV) light may be prescribed to treat patients with acute atopic dermatitis or as a maintenance therapy. Ultraviolet B (UVB), ultraviolet A (UVA), or a combination of UVB and UVA may be used during therapy.
Phototherapy can be used alone or in combination with TCS and moisturizers. Patients are encouraged to talk with their dermatologist about the risks of UV exposure (including the possible risk of skin cancer), and the ability to maintain the treatment regimen, before beginning treatment.
“While phototherapy can be very effective, it can be difficult for patients to go to a hospital or medical clinic two to three times a week as required for this treatment. If this is a significant obstacle to treatment, patients can discuss the use of home phototherapy units with their dermatologist as a convenient and cost-effective option,” said Dr. Eichenfield. - Systemic immunomodulators are indicated for patients who do not achieve adequate control of their disease through topical therapies or phototherapy or for those who have been unable to control their symptoms despite adherence to recommended treatment plans.
These therapies may also be used when a patient’s atopic dermatitis negatively affects their medical, physical and emotional well-being, especially if it impacts work, school performance or interpersonal relationships. Scientific data demonstrates that cyclosporine, methotrexate, mycophenolate and azathioprine can be effective treatments for unresponsive atopic dermatitis. Once disease is better controlled, use of systemic immunomodulators is slowly decreased. Control of atopic dermatitis is maintained through moisturizers, topical therapies, and/or phototherapy.
Treatments To Avoid
Treatments that are not recommended for patients with atopic dermatitis include
- Systemic corticosteroids as they have the potential for short- and long-term health risks and frequently lead to atopic dermatitis flares upon discontinuation. These flares can be worse than the initial flare that the therapy was trying to treat.
- Topical antihistamines should not be used as an atopic dermatitis treatment, and non-sedating antihistamines are not recommended unless there are other atopic or other allergic conditions being treated. To relieve the itchiness of atopic dermatitis that keeps a patient awake at night, a sedating antihistamine can be used on a short-term, intermittent basis, but this should not be substituted for treatment with topical therapies.
- Unless there are signs of a bacterial infection, systemic antibiotics are not recommended.
- Topical antimicrobial and antiseptic treatments, such as antibacterial soaps or bath additives are not recommended for treating atopic dermatitis and can increase the risk of a patient developing contact dermatitis.
“These guidelines provide recommendations from the latest scientific evidence available to assist in providing personalized care for atopic dermatitis patients,” said Dr. Eichenfield. “It’s especially important for patients, and parents of young patients, to follow the treatment plan prescribed by their dermatologist as this can reduce symptoms, limit disease flares, and improve the patient’s quality of life.”