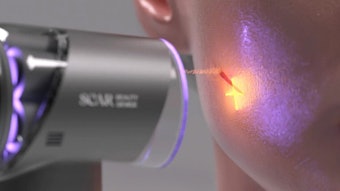
A novel dual-wavelength, dual-pulse duration laser was evaluated for use on solar lentigines in 20 Asian patients with results showing 90 percent of patients achieved moderate to significant improvement. The study device was a dual‐wavelength, dual‐pulse width Nd:YAG laser that allowed for treatment with a 532nm or 1,064 nm wavelength in a 750 picosecond pulse duration. The treating physicians used the 532nm wavelength as its effect would be confined more superficially, which is ideal for the treatment of lengitines, and because it has greater melanin absorption than 1,064nm. Furthermore, the 532nm wavelength posed less risk of adverse pigmentation events in darker skin types.
A total of 89 lesions in 20 patients were treated with the laser setting of 532nm, 750 picosecond pulse duration, fluence of 0.2–0.5 J/cm2, and spot size of 4 mm with a repetition rate of 2 Hz. The fluence was selected to achieve clinical endpoint, which was slight whitening immediately after laser shot at targeted pigment lesion. Fifty‐three of 89 (59.6 percent) lesions cleared with one laser session. Twenty‐four lesions required two treatments and 12 lesions required three treatments. Treatments were spaced 4 to 6 weeks apart.
Outcome measurements included 5-grade Physician’s Global Assessment (PGA) score, the improvement rate of relative Melanin index (MI), subjective measures of pain and overall patient satisfaction. MI was measured by reflectance spectrophotometer at baseline and at 4 and 12 weeks after final treatment. Evaluators also assessed images taken pre‐treatment, at each follow‐up visit, and at 4 and 12 weeks after final treatment, noting improvement and presence of adverse events. They evaluated pigment clearance using a 5‐grade Physician’s Global Assessment (PGA) score, where 3 represents significant improvement, 2 represents moderate improvement, 1 represents mild improvement, 0 represents no improvement, and −1 represents worsening of condition. Patient’s self‐assessment was documented at 4 and 12 weeks after final treatment using Subject Global Assessment (SGA) scale, where 3 represents significant improvement, 2 represents moderate improvement, 1 represents mild improvement, 0 represents no improvement, and −1 represents worsening of condition.
Eighteen patients (90%) achieved a moderate to significant improvement at 12‐week follow‐up based on the PGA scale. The improvement rate of relative MI (MI in the lesion minus normal skin) was 33.30 ± 18.71 and 37.63 ± 19.25% at 4‐ and 12‐week follow‐up. Post‐inflammatory hyperpigmentation (PIH) occurred in 14 of 137 sessions (10.2%), and hypopigmentation occurred in one patient with five lesions (3.6%). All cases of PIH had resolved by the 12-week follow‐up, with an average time to resolution of 6.5 weeks (3–9 weeks). One patient had hypopigmentation post‐treatment, which had resolved by 12‐week follow‐up without any intervention. One patient experienced prolonged erythema, which resolved with no medication given seven weeks following laser treatment.
The majority of patients 15 (75 percent) were satisfied to extremely satisfied with their results, with 75 percent reporting that they were likely or very likely to repeat the treatment at final follow‐up. Seventeen subjects (85 percent) said they would likely to very likely recommend this treatment to others patients.
“This work further illustrates the use of picosecond laser to treat lentigines, a most common condition among Asians. While it is effective, risk of post-inflammatory hyperpigmentation remains to be an issue and due to climate difference, it is higher than previously reported,” said lead author Henry Chan, MD, FRCP.
The full study, published in Lasers in Surgery and Medicine (June 2019), is available here.
Image Copyright Getty Images