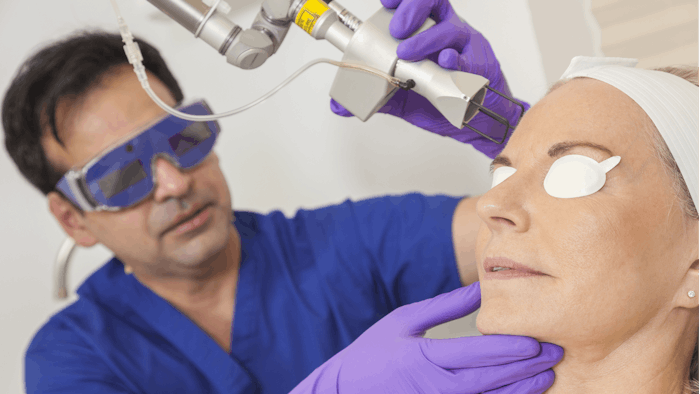
Laser and light-based devices can cause serious ocular complications, including corneal abrasions, loss of visual acuity and pupillary abnormalities. In an effort to identify risk factors and reduce the rate of ocular complications, Margit Juhasz, MD, MSc, Christopher Zachary, MD, and Joel Cohen, MD, performed a literature review of ocular complications. The results were presented by Dr. Juhasz at the 2021 ASLMS virtual conference. The study was also published in the May 2021 issue of Dermatologic Surgery.
Related: Risks of Adding Gauze to Ocular Laser Protection
The investigators searched the Pubmed/Medline Database in August 2020 for “laser and light and ocular and complication.” A total of 36 manuscripts with 94 patients were included in the review.
Of the devices cited (CO2, alexandrite, Nd:YAG, diode, argon and pulsed dye lasers and IPL), CO2 laser was, by far, the most reported as causing ocular injury when used for full-face resurfacing or periocular resurfacing.
The most common symptoms reported by patients included visual abnormality, pain, photophobia and/or erythema. The most common examination findings were ectropion, followed by uveitis, corneal abnormality, evidence of burns and pupillary abnormalities including keyhole deformity.
There also were two reported cases of bi-lateral corneal abrasions or ulcerations after corneal shields were cleansed with chlorhexidine.
Related: Laser Safety
The left eye was more often affected than the right eye. The researchers posited that this could be because providers typically stand on right side of the patient and must reach over to the left side. Therefore, they have less control of the laser when treating the left side of the face.
Dr. Juhasz shared some of the risks that lead to ocular complications during laser and light-based treatments, which include:
- The retinal hazard region is 400 nm to 1,400 nm. Because wavelengths greater than 700 nm are invisible to the naked eye, there is no blink reflex to protect the eye
- Thin eyelid skin provides little protection from light and laser
- Retinal pigment absorbs more energy than cutaneous pigment
- The palpebral oculogyric reflex (Bell phenomenon), in which the eye rolls up when the eye is closed brings the pigmented structures of the eye into closer proximity with laser or light sources
Lack of Eye Protection Reported
Only 12.8% of the cases reported use of eye protection at the time of injury, and 28.7% reported that no eye protection was used, eyes were closed or fingers were placed over eyes during treatment.
When reviewing lawsuits related to ocular damage (2.2% of lawsuits following laser or light treatments are due to ocular injury), lack of informed consent was the most common cause of the suit.
The review also revealed that 66.6% of the injuries were due to operator error (lacking protective eyewear and/or deviating from safety protocol), and 57.5% named a physician as the operator.
Factors Affecting Ocular Injuries
There are several factors that affect the risk or rate of ocular injury including:
- Duration of exposure and distance from exposure
- Eye color (light more likely to experience retinal injury; dark more likely to experience pupillary abnormality)
- Pupil size (2-3mm)
- High visual acuity
- History of prior ocular aberrations
How To Prevent Injuries
There are several steps that practitioners can take to reduce the risk of ocular injury. Prior to treatment, exogenous materials, such as mascara—which increases energy absorption—should be removed. Patients should use eye protection. The gold standard being metal corneal shields. “Do not treat inside the orbital rim without metal corneal shields,” said Dr. Juhasz.
Practitioners should be trained in and follow safety protocols, including the use of signage when a laser is in use and not opening and closing doors during a procedure. In addition, laser operators should be trained in early recognition of the signs and symptoms of ocular injury.