For their paper published by the Journal of Cosmetic Dermatology (August 11, 2021), Mark S. Nestor, MD, PhD, et al, performed a literature review to highlight the rates, causes and management of blepharoptosis (eyelid ptosis) secondary to botulinum toxin type A (BoNT-A) injections. The review also highlights new anatomic pathways through which BoNT-A may spread from the brow area to the levator palpebrae superioris muscle.
Related: Achieving Longer-Lasting Botulinum Toxin Treatments
The authors conducted a literature search using electronic databases (PubMed, Science Direct, MEDLINE, Embase, CINAHL, EBSCO) regarding eyelid anatomy and the underlying pathogenesis, presentation, prevention and treatment of eyelid ptosis secondary to BoNT-A. They also perfomed anatomic dissection to assess the role of neurovascular pedicles and supraorbital foramen anatomic variations.
Rates of blepharoptosis following BoNT-A injections—which occurs due to weakness of the levator palpebrae superioris muscle—are estimated to be 5.4% among inexperienced injectors and <1% among experienced injectors. Mean onset is three to 14 days after injection and eventually self-resolves after the paralytic effect of BoNT-A wanes.
Related: Comparing Btx Injection Techniques for Axillary Hyperhidrosis
Blepharoptosis occurs when the levator palpebrae superioris (LPS) muscle is weakened in the superior intraorbital compartment due to BoNT-A. Though the superficial frontal (third facial anatomic layer) and deep intraorbital (deep to the facial fifth layer) are separated by the fibrous orbital septum, an anatomic barrier, the researchers identified a few weak points that could allow for unintended spread of toxin: the superior neurovascular pedicles (ie, supratrochlear, supraorbital and lacrimal pedicles).
In addition, the anatomic study showed that a supraorbital foramen may be present in some patients, constituting a shortcut from the brow area directly into the orbital roof, following the supraorbital neurovascular pedicle.
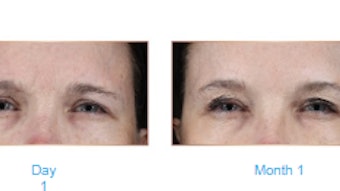
If eyelid ptosis occurs, administration of medications, such as oxymetazoline hydrochloride or apraclonidine hydrochloride eye drops, anticholinesterase agents, or transdermal BoNT-A injections to the pre-tarsal orbicularis, can at least partially reverse it.