The quilting technique, a method originating in Brazil, is not new to U.S. facelift procedures, initially used internally, beneath the skin after finishing a facelift to eliminate the potential space created between the layers of tissues. Most recently, however, the procedure has gained attraction for external quilting, or “hemostatic netting,” especially as surgeons increasingly practice facelifts compared to previous years since the rise of GLP-1 use and preventive aesthetics. The use of this technique for traditional and deep plane facelifts has grown as the number of procedures grow–shown to reduce the incidence of post-surgical bleeding, also known as hematoma, and also the amount of tension on the skin and risk of skin compromise, or necrosis.
As More Patients Seek Early Intervention, External Quilting Offers a Modern Fix for a Classic Procedure
On average, members of the American Academy of Facial Plastic and Reconstructive Surgery performed 48 facelifts or partial facelifts in 2023, demonstrating a 60% increase since 2017 [1]. About 32% of AAFPRS patients seeking facelifts are now ages 35-55 [2], suggesting that facelift patients are getting younger as they seek steps to prevent aging and preserve their youth before it occurs, and also as an increasing number of patients experience the “Ozempic effect” [1].
“By reducing [post surgical bleeding and skin compromise], healing is expedited [with quilting] and leads to improvement in the appearance of the surgical incisions,” says Gina Maccarone, MD, FACS, the founder of the Surgeonista, who specializes in facelifts.
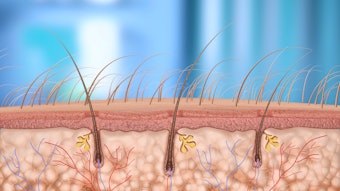
The quilting technique, or hemostatic netting, places sutures on the skin’s exterior to anchor it to the underlying fascia, eliminating the use of external drains to manage fluid buildup and prevent a common result of facelifts: hematoma. Maccarone says external quilting has become a popular technique over internal because external netting can be more efficient, requiring less time to place than internal sutures. Sometimes, too, the expense of the suture type is also considered, and external netting sutures are often inexpensive compared to certain sutures that are used internally. However, the techniques depend on surgeon preference, and both are considered fairly equal in efficacy.
 About 32% of AAFPRS patients seeking facelifts are now ages 35-55, suggesting that facelift patients are getting younger as they seek steps to prevent aging and preserve their youth before it occurs, and also as an increasing number of patients experience the “Ozempic effect.”Courtesy of Yuliia at Adobe Stock
About 32% of AAFPRS patients seeking facelifts are now ages 35-55, suggesting that facelift patients are getting younger as they seek steps to prevent aging and preserve their youth before it occurs, and also as an increasing number of patients experience the “Ozempic effect.”Courtesy of Yuliia at Adobe Stock
Hemostatic Netting Cuts Post-Facelift Bleeding Rates Dramatically—A Safer Alternative to Drains and Dressings
A hematoma, occurring in up to to 14.2% of face and neck lift procedures [3], is a localized collection of blood outside of blood vessels that results in swelling, discoloration and sometimes airway obstruction and skin necrosis. By eliminating external drains to manage fluid buildup, quilting sutures reduce discomfort and speed up the recovery process, says Konstantin Vasyukevich, MD, who practices quilting.
In a 2023 study, the rate of hematoma incidences in a series of facelifts was 3.6%, improving to an incidence of 0.6% among patients with the use of hemostatic netting, also known as external quilting,[3].
Hemostatic netting has shown to reduce post-operative bleeding to the lowest incidence possible when compared to other methods, Maccarone says. Other options include drain usage, which doesn’t reduce bleeding, she adds, and simply alerts the patient and surgeon more quickly when it does occur. External compression with a bandage, on the other hand, or use of a topical solution on the operative surface that reduces bleeding is another method to address bleeding, but is also not as successful as quilting.
The sutures are placed through the skin into the deeper tissue, Vasyukevich explains. As long as the minimal tension is maintained, these sutures are unlikely to cause visible marks or scarring. There is a very small risk of pinpoint scar formation at any of the entry sites for the quilting, but these fade and improve with time, Maccarone adds.
“However, in a situation of significant tissue edema (swelling) or fluid collection, excessive tension from the sutures could lead to tissue damage and potential scaring,” Vasyukevich says.
Despite Visible Stitches, Quilting Poses No Added Risk or Downtime When Performed by Skilled Surgeons
When the procedure is done by a surgeon with the correct experience and understanding of face anatomy, Maccarone says quilting does not create any additional inconvenience to the patient other than the temporary external appearance that creates a stitch resembling a net or quilt. The technique eliminates the potential complication or a return to emergent surgery, making it a good option for creating optimal results without any notable additional risk, she adds.
The short term appearance of the technique, due to the sutures being placed externally, often leads to anxiety for patients. However, Maccarone says, they are removed at the follow up appointment after surgery, during the normal period of downtime after this operation, so there is no change in the normal time frame for recovery.
Over time, Maccarone says the technique enhances the facelift results by avoiding the potential for complications and helps maintain the integrity of the tissues in a more reliable way.
Quilting Isn’t One-Size-Fits-All: Surgeon Skill and Skin Type Matter in Achieving Optimal Facelift Outcomes
“This technique is not specific for a particular facial structure; however, one would be well advised to exercise caution in patients with darker skin types to avoid visible skin marks,” Vasyukevich says.
As facelift success, especially deep planes that take more time and precision, as well as quilting technique varies by surgeon expertise and experience, it’s important to consult with the surgeon to discuss your needs to avoid complications and determine if this method is right for your aesthetic and medical goals.
References:
2- https://www.aafprs.org/Media/Press_Releases/2024_Annual_Trends_Survey.aspx